Conditions And Symptoms We Treat
- Achilles Tendonitis
The Achilles tendon is the largest tendon in the human body and can withstand forces of 1,000 pounds or more. It also is the most frequently ruptured tendon, usually as a result of a sports injury. Both professional and weekend athletes may suffer from Achilles tendonitis, a common overuse injury and inflammation of the tendon.
Events that can cause Achilles tendonitis may include:
- Hill running or stair climbing.
- Overuse, stemming from the natural lack of flexibility in the calf muscles.
- Rapidly increasing mileage or speed when walking, jogging, or running.
- Starting up too quickly after a layoff in exercise or sports activity, without adequately stretching and warming up the foot.
- Trauma caused by sudden and/or hard contraction of the calf muscles when putting out extra effort, such as in a sprint.
- Improper footwear and/or a tendency toward overpronation.
Achilles tendonitis often begins with mild pain after exercise or running that gradually worsens. Other symptoms include:
- Recurring localized pain, sometimes severe, along the tendon during or a few hours after running.
- Morning tenderness about an inch and a half above the point where the Achilles tendon is attached to the heel bone.
- Sluggishness in your leg.
- Mild or severe swelling.
- Stiffness that generally diminishes as the tendon warms up with use.
Treatment normally includes:
- A bandage specifically designed to restrict motion of the tendon.
- Taking nonsteroidal anti-inflammatory medication for a period of time. Note: Please consult your physician before taking any medication.
- Orthotics, which are corrective shoe inserts designed to help support the muscle and relieve stress on the tendon. Both nonprescription orthoses (such as a heel pads or over-the-counter shoe inserts) and prescribed custom orthotics may be recommended depending on the length and severity of the problem.
- Rest and switching to exercises that do not stress the tendon (such as swimming).
- Stretching and exercises to strengthen the weak muscle group in front of the leg, calf, and the upward foot flexors, as well as massage and ultrasound.
- In extreme cases, surgery is performed to remove the fibrous tissue and repair any tears.
- Ankle Sprain
Ankle sprains are caused by an unnatural twisting or force on the ankle bones of the foot, which may result in excessive stretching or tearing of one or more ligaments on the outside of the ankle. The severity of the sprain can impact the degree of damage as well as the type and duration of treatment. If not properly treated, ankle sprains may develop into long-term problems.
Primary symptoms of ankle sprains are pain following a twist or injury, swelling, and bruising.
Treatment includes resting and elevating the ankle and applying ice to reduce swelling. Compressive bandages also may be used to immobilize and support the injury during healing. Serious ankle sprains, particularly among competitive athletes, may require surgery to repair and tighten the damaged ligaments.
To prevent ankle sprains, try to maintain strength, balance, and flexibility in the foot and ankle through exercising, stretching, and wearing well-fitted shoes.
- Arthritis
Arthritis is an inflammation and swelling of the cartilage and lining of the joints, generally accompanied by an increase in the fluid in the joints. Arthritis is a disabling and occasionally crippling disease afflicting almost 40 million Americans. In some forms, it appears to be hereditary. Although the prevalence of arthritis increases with age, all people from infancy to middle age are potential victims. People over 50 are the primary targets.
If the feet seem more susceptible to arthritis than other parts of the body, it is because each foot has 33 joints that can be afflicted, and there is no way to avoid the pain of the tremendous weight-bearing load on the feet. Arthritic feet can result in loss of mobility and independence. However, early diagnosis and proper medical care can limit or slow the damage.
Symptoms of arthritis in the foot and ankle include:
- Early morning stiffness.
- Limitation in motion of joint.
- Recurring pain or tenderness in any joint.
- Redness or heat in a joint.
- Skin changes, including rashes and growths.
- Swelling in one or more joints.
Forms of Arthritis
Osteoarthritis is the most common form of arthritis. It is frequently called degenerative joint disease or wear and tear arthritis. Aging usually brings on a breakdown in cartilage, and pain gets progressively more severe. Dull, throbbing nighttime pain is characteristic, and may be accompanied by muscle weakness or deterioration. Many of these symptoms can be relieved with rest. Overweight people are particularly susceptible to osteoarthritis. The additional weight contributes to the deterioration of cartilage and the development of bone spurs.
Rheumatoid arthritis is a major crippling disorder and the most serious form of arthritis. It is a complex, chronic inflammatory group of diseases, often affecting more than a dozen smaller joints during its course. In the foot, it frequently affects both ankles and toes.
Arthritis of the foot and ankle can be treated in many ways, including:
- Physical therapy and exercise.
- Anti-inflammatory medication and/or steroid injections into the affected joint. Note: Please consult your physician before taking any medications.
- Orthotics or specially prescribed shoes.
- Bunions
A bunion is a bone deformity caused by an enlargement of the joint at the base and side of the big toe (metatarsophalangeal joint). Bunions form when the toe moves out of place. The enlargement and its protuberance cause friction and pressure as they rub against footwear. Over time, the movement of the big toe angles in toward the other toes, sometimes overlapping a third toe (known as Hallux Valgus). The growing enlargement or protuberance then causes more irritation or inflammation. In some cases, the big toe moves toward the second toe and rotates or twists, which is known as Hallus Abducto Valgus. Bunions can also lead to other toe deformities, such as hammertoe.
Many people with bunions suffer from discomfort and pain from the constant irritation, rubbing, and friction of the enlargement against shoes. The skin over the toe becomes red and tender. Because this joint flexes with every step, the bigger the bunion gets, the more it hurts to walk. Over time, bursitis or arthritis may set in, the skin on the bottom of the foot may become thicker, and everyday walking may become difficult—all contributing to chronic pain.
Wearing shoes that are too tight is the leading cause of bunions. Bunions are not hereditary, but they do tend to run in families, usually because of a faulty foot structure. Foot injuries, neuromuscular problems, flat feet, and pronated feet can contribute to their formation. It is estimated that bunions occur in 33 percent of the population in Western countries.
Treatment for Bunions
Because they are bone deformities, bunions do not resolve by themselves. The goal for bunion treatment is twofold: first, to relieve the pressure and pain caused by irritations, and second to stop any progressive growth of the enlargement. Commonly used methods for reducing pressure and pain caused by bunions include:
- Protective padding, often made from felt material, to eliminate the friction against shoes and help alleviate inflammation and skin problems.
- Removal of corns and calluses on the foot.
- Changing to carefully fitted footwear designed to accommodate the bunion and not contribute toward its growth.
- Orthotic devices—both over-the-counter and custom made—to help stabilize the joint and place the foot in the correct position for walking and standing.
- Exercises to maintain joint mobility and prevent stiffness or arthritis.
- Splints for nighttime wear to help the toes and joint align properly. This is often recommended for adolescents with bunions, because their bone development may still be adaptable.
Surgical Treatment
Depending on the size of the enlargement, misalignment of the toe, and pain experienced, conservative treatments may not be adequate to prevent progressive damage from bunions. In these cases, bunion surgery, known as a bunionectomy, may be advised to remove the bunion and realign the toe.
- Corns and Calluses
Corns and calluses are protective layers of compacted, dead skin cells. They are caused by repeated friction from skin rubbing against bony areas or against an irregularity in a shoe. Corns ordinarily form on the toes and calluses on the soles of the feet. The friction and pressure can burn or otherwise be painful and may be relieved by moleskin or padding on the affected areas.
Never cut corns or calluses with any instrument, and never apply home remedies, except under a podiatrist’s instructions.
- Diabetic Care
According to the American Diabetes Association, about 15.7 million people (5.9 percent of the United States population) have diabetes. Nervous system damage (also called neuropathy) affects about 60 to 70 percent of people with diabetes and is a major complication that may cause diabetics to lose feeling in their feet or hands.
Foot problems are a big risk in diabetics. Diabetics must constantly monitor their feet or face severe consequences, including amputation.
With a diabetic foot, a wound as small as a blister from wearing a shoe that’s too tight can cause a lot of damage. Diabetes decreases blood flow, so injuries are slow to heal. When your wound is not healing, it’s at risk for infection. As a diabetic, your infections spread quickly. If you have diabetes, you should inspect your feet every day. Look for puncture wounds, bruises, pressure areas, redness, warmth, blisters, ulcers, scratches, cuts and nail problems. Get someone to help you, or use a mirror.
Here’s some basic advice for taking care of your feet:
- Always keep your feet warm.
- Don’t get your feet wet in snow or rain.
- Don’t put your feet on radiators or in front of the fireplace.
- Don’t smoke or sit cross-legged. Both decrease blood supply to your feet.
- Don’t soak your feet.
- Don’t use antiseptic solutions, drugstore medications, heating pads or sharp instruments on your feet.
- Trim your toenails straight across. Avoid cutting the corners. Use a nail file or emery board. If you find an ingrown toenail, contact our office.
- Use quality lotion to keep the skin of your feet soft and moist, but don’t put any lotion between your toes.
- Wash your feet every day with mild soap and warm water.
- Wear loose socks to bed.
- Wear warm socks and shoes in winter.
- When drying your feet, pat each foot with a towel and be careful between your toes.
- Buy shoes that are comfortable without a “breaking in” period. Check how your shoe fits in width, length, back, bottom of heel, and sole. Avoid pointed-toe styles and high heels. Try to get shoes made with leather upper material and deep toe boxes. Wear new shoes for only two hours or less at a time. Don’t wear the same pair every day. Inspect the inside of each shoe before putting it on. Don’t lace your shoes too tightly or loosely.
- Choose socks and stockings carefully. Wear clean, dry socks every day. Avoid socks with holes or wrinkles. Thin cotton socks are more absorbent for summer wear. Square-toes socks will not squeeze your toes. Avoid stockings with elastic tops.
When your feet become numb, they are at risk for becoming deformed. One way this happens is through ulcers. Open sores may become infected. Another way is the bone condition Charcot (pronounced “sharko”) foot. This is one of the most serious foot problems you can face. It warps the shape of your foot when your bones fracture and disintegrate, and yet you continue to walk on it because it doesn’t hurt. Diabetic foot ulcers and early phases of Charcot fractures can be treated with a total contact cast.
The shape of your foot molds the cast. It lets your ulcer heal by distributing weight and relieving pressure. If you have Charcot foot, the cast controls your foot’s movement and supports its contours if you don’t put any weight on it. To use a total contact cast, you need good blood flow in your foot. The cast is changed every week or two until your foot heals. A custom-walking boot is another way to treat your Charcot foot. It supports the foot until all the swelling goes down, which can take as long as a year. You should keep from putting your weight on the Charcot foot. Surgery is considered if your deformity is too severe for a brace or shoe.
- Foot Odor
The feet and hands contain more sweat glands than any other part of the body, with roughly 3,000 glands per square inch. Smelly feet are not only embarrassing, but can be physically uncomfortable as well.
Feet smell for two reasons: 1) shoe wear, and 2) sweating of the feet. The interaction between the perspiration and the bacteria that thrive in shoes and socks generates the odor. Therefore, any attempt to reduce foot odor has to address both sweating and footwear.
Smelly feet or excessive sweating can also be caused by an inherited condition, called hyperhidrosis, which primarily affects men. Stress, some medications, fluid intake, and hormonal changes also can increase the amount of perspiration our bodies produce.
In general, smelly feet can be controlled with a few preventive measures:
- Always wear socks with closed shoes.
- Avoid wearing nylon socks or plastic shoes. Instead, wear shoes made of leather, canvas, mesh, or other materials that let your feet breathe.
- Bathe feet daily in lukewarm water, using a mild soap. Dry thoroughly.
- Change socks and shoes at least once a day.
- Check for fungal infections between toes and on the bottoms of your feet. If any redness or dry, patchy skin is observed, get treatment right away.
- Don’t wear the same pair of shoes two days in a row. If you frequently wear athletic shoes, alternate pairs so that the shoes can dry out. Give your shoes at least 24 hours to air out between wearings; if the odor doesn’t go away, discard the shoes.
- Dust your feet frequently with a nonmedicated baby powder or foot powder. Applying antibacterial ointment also may help.
- Practice good foot hygiene to keep bacteria levels at a minimum.
- Wear thick, soft socks to help draw moisture away from the feet. Cotton and other absorbent materials are best.
Treating Foot Odor
The best home remedy for foot odor is to soak feet in strong black tea for 30 minutes a day for a week. The acid in the tea kills the bacteria and closes the pores, keeping your feet dry longer. Use two tea bags per pint of water. Boil for 15 minutes, then add two quarts of cool water. Soak your feet in the cool solution. Alternately, you can soak your feet in a solution of one part vinegar and two parts water.
Persistent foot odor can indicate a low-grade infection or a severe case of hereditary sweating. In these cases, a prescription ointment may be required to treat the problem.
Treating Excessive Sweating
A form of electrolysis, called iontophoresis, has been shown to reduce excessive sweating of the feet. However, it is more difficult to administer. In the worst cases of hyperhidrosis, a surgeon can cut the nerve that controls sweating. Recent advances in technology have made this surgery much safer, but may increase sweating in other areas of the body.
- Fractures of the Foot/Ankle
Nearly one-fourth of all the bones in your body are in your feet. A broken (fractured) bone in your forefoot or in one of your toes is often painful, but rarely disabling. Most of the time, these injuries heal without operative treatment.
There are two types of foot fractures: stress fractures and general bone fractures. Stress fractures usually occur in the bones of the forefoot extending from the toes to the middle of the foot. Stress fractures are like tiny cracks in the bone surface. They can happen with sudden increases in exercise (such as running or walking for longer distances or times), improper training techniques, or a change in surfaces.
Most other types of fractures extend through the bone, and are called bone fractures. They may be stable, in which there is no shift in bone alignment, or displaced, in which the bone ends no longer line up properly. Bone fractures usually result from trauma, such as dropping a heavy object on your foot, or from a twisting injury. If the fractured bone does not break through the skin, it is called a closed fracture. If the fracture does break through the skin, it is called an open fracture.
Because of the complex structures in the foot, there are some other, more specific types of fractures that can occur. For example, the fifth metatarsal, known as the little or pinky toe, is susceptible to a variety of different fractures. The relationship between the ankle and the foot can be compromised by an ankle-twisting injury, which may tear the tendon that attaches to this bone and pull a small piece of the bone away. A more serious injury in the same area is known as a Jones fracture, which occurs near the base of the bone and disrupts its blood supply. This injury may take longer to heal or require surgery.
Common symptoms for any type of foot fracture includes pain, swelling, and sometimes bruising. Be sure to seek medical attention for any suspected foot fracture
- Hammertoes
Hammertoe is a deformity of the second, third, or fourth toes. In this condition, the toe is bent at the middle joint, causing it to resemble a hammer. Left untreated, hammertoes can become inflexible and require surgery. People with hammertoe may have corns or calluses on the top of the middle joint of the toe or on the tip of the toe. They may also feel pain in their toes or feet and have difficulty finding comfortable shoes.
Causes of hammertoe include improperly fitting shoes and muscle imbalance.
Treatment for the condition typically involves wearing shoes with soft, roomy toe boxes and toe exercises to stretch and strengthen the muscles. Commercially available straps, cushions, or nonmedicated corn pads may also relieve symptoms.
In severe cases, hammertoe surgery may be recommended to correct the deformity.
- Heel Pain
Heel pain is caused by many different conditions. The most common type of heel pain occurs on the bottom of the heel and is caused by inflammation in a ligament called the plantar fascia. The pain in this condition is located on the middle bottom of the heel or along the back of the arch where it meets the heel, and is usually present in most people upon first arising in the morning or after arising from a seated position. Plantar fasciitis, as it is called, is seen in those with flat feet and in those with high arches. Flat feet, which are usually the cause of this condition, allow for chronic stretching and tearing of the fascia where it attaches to the heel bone. The foot does not have to be severely flat for this to occur, as moderate flattening can cause damage also. High arches, another common cause, allow for abnormal shock to be transmitted to the heel with every step. Direct injuries or traumatic tearing of the tissue (either miniscule, partial, or complete), though less common, can also cause inflammation to the plantar fascia. Though possibly self-healing over a long period of time, this condition can last for many years when no treatment is given, and can make activity nearly impossible. For treatment, a combination therapy of inflammation reduction with anti-inflammatory medications, steroid injections, icing and stretching is necessary, along with arch support through prescription shoe inserts (orthotics) to stabilize and support a flat foot or provide shock absorption to a high arched foot. Only rarely is surgery required.
Inflammation control will reduce the pain, and help heal the injury as long as it has not reached a chronic stage of scarring and ongoing inflammation called fasciosis. This is seen in fasciitis cases that do not get treated for a long while. The use of a steroid injection (cortisone-like medication, not a bodybuilding steroid) seems to have the most immediate impact on patients, although the reduction in inflammation can take up to a week to occur after the injection and up to three injections may be needed, best split two weeks apart. Anti-inflammatory medications, like strong prescription versions of ibuprofen, also help reduce the body’s overall state of inflammation, reducing pain further. Finally, icing of the arch and heel to decrease more inflammation will be necessary, as well as stretching of the arch and calf to make the bottom of the foot more limber, reducing damage to the fascia.
Pain behind the heel can usually be caused by inflammation of the Achilles tendon (tendonitis), as well as inflammation due to extra bone growth in the heel bone (Haglund’s deformity and heel spurs). Achilles tendonitis is quite common, and activity only worsens the condition. It develops for a wide variety of reasons. These include chronic stretching of the tendon from unbalanced motion, violent injuries forcing the foot upward, and blunt pressure on the back of the heel itself as when someone steps on another’s heel. When combined with a spur or enlargement of the back of the heel bone, even simple shoe use can be painful as the heel rubs against the back of the shoe. The pain can feel dull, sharp and knife-like, throbbing, aching, or all of the above. This pain usually goes down with rest and inactivity, and resumes with simple motion at the ankle or full activity.
Treatment centers around stretching of the Achilles tendon, along with icing, anti-inflammatory medication, ankle bracing, and physical therapy. A tight Achilles tendon makes recovery incredibly difficult, and stretching becomes the most important aspect of this treatment course. Icing and anti-inflammatory medication relieve the inflamed tissue around and in the tendon, and bracing prevents excessive tendon pulling. This will all help to reduce pain and improve mobility, as well as foster full healing. When needed, physical therapy accomplishes numerous goals, including eventual inflammation reduction, improved flexibility, and better tendon strength. Immobilization in a walking cast, or with a non-weight bearing cast with crutches may be necessary in severe cases. Unfortunately, many people ignore their pain until it is very advanced. Untreated Achilles tendonitis can lead to tendon degeneration and even rupture. This requires surgical repair in many cases. When the bone spur or bone enlargement is causing most of the pain, and the treatment outlined above is not helping, surgery is needed to remove the excess bone to relieve pressure off the Achilles tendon. This procedure requires the most surgical recovery time and needs nearly 3 months rehabilitation prior to returning to activity.
- Ingrown Toenails
Ingrown nails are nails whose corners or sides dig painfully into the skin, often causing infection. They are frequently caused by improper nail trimming, but also by shoe pressure, injury, fungus infection, heredity, and poor foot structure.
Toenails should be trimmed straight across, slightly longer than the end of the toe, with toenail clippers.
- Orthotics
Orthotics, also known as orthoses, refers to any device inserted into a shoe, ranging from felt pads to custom-made shoe inserts that correct an abnormal or irregular, walking pattern. Sometimes called arch supports, orthotics allow people to stand, walk, and run more efficiently and comfortably. While over-the-counter orthotics are available and may help people with mild symptoms, they normally cannot correct the wide range of symptoms that prescription foot orthoses can since they are not custom made to fit an individual’s unique foot structure.
Orthotic devices come in many shapes, sizes, and materials and fall into three main categories: those designed to change foot function, those that are primarily protective in nature, and those that combine functional control and protection.
Rigid Orthotics
Rigid orthotic devices are designed to control function and are used primarily for walking or dress shoes. They are often composed of a firm material, such as plastic or carbon fiber. Rigid orthotics are made from a mold after a podiatrist takes a plaster cast or other kind of image of the foot. Rigid orthotics control motion in the two major foot joints that lie directly below the ankle joint and may improve or eliminate strains, aches, and pains in the legs, thighs, and lower back.
Soft Orthotics
Soft orthotics are generally used to absorb shock, increase balance, and take pressure off uncomfortable or sore spots. They are usually effective for diabetic, arthritic, and deformed feet. Soft orthotics are typically made up of soft, cushioned materials so that they can be worn against the sole of the foot, extending from the heel past the ball of the foot, including the toes. Like rigid orthotics, soft orthotics are also made from a mold after a podiatrist takes a plaster cast or other kind of image of the foot.
Semi-Rigid Orthotics
Semi-rigid orthotics provide foot balance for walking or participating in sports. The typical semi-rigid orthotic is made up of layers of soft material, reinforced with more rigid materials. Semi-rigid orthotics are often prescribed for children to treat flatfoot and in-toeing or out-toeing disorders. These orthotics are also used to help athletes mitigate pain while they train and compete.
- Plantar Fasciitis
Plantar fasciitis is the term commonly used to refer to heel and arch pain traced to an inflammation on the bottom of the foot. More specifically, plantar fasciitis is an inflammation of the connective tissue, called plantar fascia, that stretches from the base of the toes, across the arch of the foot, to the point at which it inserts into the heel bone. Overpronation is the most common cause of plantar fasciitis. As the foot rolls inward excessively when walking, it flattens the foot, lengthens the arch, and puts added tension on the plantar fascia. Over time, this causes inflammation.
Also known as heel spur syndrome, the condition is often successfully treated with conservative measures, such as the use of anti-inflammatory medications, ice packs, stretching exercises, orthotic devices, and physical therapy.
- Plantar Warts
Most foot warts are harmless, even though they may be painful. They are often mistaken for corns or calluses, which are layers of dead skin that build up to protect an area which is being continuously irritated. A wart, however, is caused by a viral infection which invades the skin through small or invisible cuts and abrasions. Foot warts are generally raised and fleshy and can appear anywhere on the foot or toes. Occasionally, warts can spontaneously disappear after a short time, and then, just as frequently, they recur in the same location. If left untreated, warts can grow to an inch or more in circumference and can spread into clusters of warts. Children, especially teenagers, tend to be more susceptible to warts than adults.
Plantar warts, also known as verrucas, appear on the soles of the feet and are one of several soft tissue conditions that can be quite painful. Unlike other foot warts, plantar warts tend to be hard and flat, with a rough surface and well-defined boundaries. They are often gray or brown (but the color may vary), with a center that appears as one or more pinpoints of black. Plantar warts are often contracted by walking barefoot on dirty surfaces or littered ground. The virus that causes plantar warts thrives in warm, moist environments, making infection a common occurrence in public pools and locker rooms.
Like any other infectious lesion, plantar warts are spread by touching, scratching, or even by contact with skin shed from another wart. The wart may also bleed, another route for spreading. Plantar warts that develop on the weight-bearing areas of the foot (the ball or heel of the foot) can cause a sharp, burning pain. Pain occurs when weight is brought to bear directly on the wart, although pressure on the side of a wart can create equally intense pain.
To prevent the spread of warts, follow these tips:
- Avoid direct contact with warts, both from other persons or from other parts of the body.
- Avoid walking barefoot, except on sandy beaches.
- Change your shoes and socks daily.
- Check your children’s feet periodically.
- Keep your feet clean and dry.
It is important to note that warts can be very resistant to treatment and have a tendency to reoccur. Over-the-counter foot wart treatments are usually ineffective because their use can inadvertently destroy surrounding healthy tissue. Please contact our office for help in effectively treating warts. Our practice is expert in recommending the best treatment for each patient, ranging from prescription ointments or medications to, in the most severe cases, laser cautery.
- Sports Injuries
Many sports are hard on the feet because of quick repetitive movements, constricting footwear, and/or increased exposure to injury or trauma. Following is a brief overview of some of the most common injuries that result from particular sports.
Martial Arts and Kick Boxing
Injuries commonly seen as a result of martial arts and kick boxing include plantar fasciitis, Achilles tendonitis, sesamoiditis, and ankle sprains. Stretching is recommended to help prevent injury: specifically, a minimum of 15 minutes of stretching before performing any kicking or punching.
Aerobics
Impact forces from aerobics can reach up to six times the force of gravity, which is transmitted to each of the 26 bones in the foot. That is why proper shoes are crucial to successful, injury-free aerobics. Shoes should provide sufficient cushioning and shock absorption to compensate for pressure on the foot many times greater than found in walking. They must also have good medial-lateral stability.
Team Sports
Activities such as football, baseball, basketball, soccer, field hockey, and lacrosse often lead to ankle injuries as a result of play on artificial surfaces, improper footwear, and/or inadequate stretching.
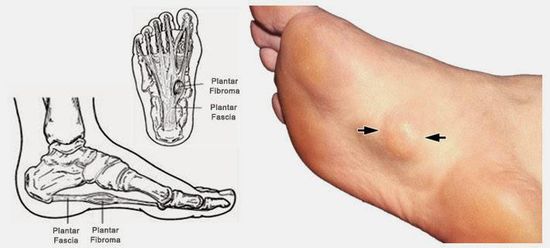
INFORMATION ABOUT PLANTAR FIBROMATOSIS
Mon -Thu 8:30 am - 4:30 pm
Friday 8:30 am - 3:30 pm - Lunch 12:00 pm -1 :30 pm
Mon -Thu 8:30 am - 4:30 pm
Friday 8:30 am - 3:30 pm - Lunch 12:00 pm -1 :30 pm
Nexton Office
1229 Nexton Pkwy, Unit C3, Summerville 29486
Mon -Thu 8:30 am - 4:30 pm
Friday 8:30 am - 3:30 pm - Lunch 12:00 pm -1 :30 pm






- Main Office 4340 Ladson Rd, Ladson, SC 29456, United States
- North Charleston Office 2891 Tricom St, North Charleston, SC 29406, United States
- Moncks Corner Office 730 Stony Landing Rd, Moncks Corner, SC 29461, United States
- Summerville Medical Center 295 Midland Pkwy, Summerville, SC 29485, United States
- Charleston Surgery Center Edge St, Summerville, SC, United States
- Nexton Office Nexton Pkwy, Summerville, SC 29486, United States of America